Pathology Lab Field Trip: A Visit with One of the “Hidden Heroes” (Part Two of Two)
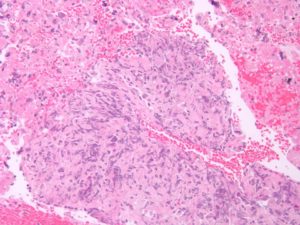
Recently, I visited Dr. Charles Lombard, the Medical Director of Pathology at El Camino Hospital, where I was able to see slides of my biopsied cancer cells and tour the lab (see my discussion and pics in my blog Field Trip to the Pathology Lab! (Part One of Two)).
Although I enjoyed seeing my cancer slides and the lab, that was not the most remarkable part of my field trip. During my conversation with Dr. Lombard, the man who signed my pathology report, he mentioned that he personally had lobbied for and gotten approval for testing lung biopsies in his lab for ROS1, starting on January 1, 2014. I had my biopsy on January 10, 2014. Whoa. It would be hard to overstate how critical this seemingly minor administrative detail was for me. Learning of my ROS1+ status dramatically shifted my treatment plan and survival curve. If I had had my biopsy just 10 days earlier, I may not have been sitting in his office that afternoon. *Please take a moment to reread that last sentence and let it sink in.*
I regularly marvel at the miracle: amidst this mess, I landed in a hospital that tested for ROS1 before I even had a chance to learn about and ask for it – before there was even an FDA approved therapy for ROS1+ patients. Even today, 3.5 years later, testing for ROS1 is not the standard of care for most hospitals in the U.S., and even less common outside the U.S. Many patients either never learn of their ROS1+ status, or learn of it too late.
Not only am I struck by my luck, but I am struck that this was all invisible to me. I took great care in choosing my pulmonologist and surgeon and later my oncologist, but I paid no mind whatsoever to who would be my pathologist, or the quality of the pathology lab. It didn’t even occur to me to inquire about pathology until more than 3 years after the fact.
This issue has come up once before for me, in a slightly different context. Although I get lab work and check-in with my oncologist once a month, the crux of my care turns on my scan reports every 2-4 months. Every single treatment decision hinges on what my scan report says; no other measure even comes close as a diagnostic tool. And who writes these reports? A revolving staff of radiologists whom I’ve never met. I live or die by these reports, but I have no idea who is writing them, and they have no idea who I am either. I am a patient file number, in a stack of hundreds of other patient file numbers.
I was so struck by this realization last year that I brought it up with my oncologist. “Can I possibly meet the radiologist? Could I at least request that the same radiologist read my scans each time, so there’s consistency?” My oncologist, humoring his pain-in-the-ass patient, tried to accommodate me, but as it turns out, the answer was essentially, “no.” The system is just not set up that way. Radiologists are usually off-site, and they work as a team. Whoever reads your scans is whoever is on-duty at the time; it is not efficient to have them assigned to particular patients.
As a patient, I try very hard to take an active, responsible, role in my own care. I am not a scientist. I defer to my doctors’ expertise. But, I do not hand over the reins completely. I spend time educating myself about my condition and I make decisions about my doctors and treatments with care. It makes me somewhat uncomfortable that two of the most critical functions in my care team – pathology and radiology – operate completely apart from and invisible to patients.
I am not quite sure what to do about my discomfort. I understand that healthcare is a vast and complex system and it is not practical for patients to be involved at every level. On the other hand, patients are often counseled to advocate for themselves, not lose their sovereignty. Moreover, I cannot shake my gut sense that it is human nature for a doctor to take a little more care with a patient s/he has some familiarity with (and studies like this one bear this out). I haven’t figured out any real solutions to truly resolve my discomfort. It is a delicate balance. A dance. At least I’m learning more about the boundaries – where patients may get more involved (and push into places like basement path labs), and where we must simply trust.
Luckily, there are hidden heroes – like pathologists lobbying for ROS1 testing for patients they don’t even know and radiologists who haven’t failed me yet (despite the fact that I haven’t figured out how to crash their offices thus far). At least it feels better to me to be learning what I don’t or can’t know, and how important things happen behind the scenes. And it was pretty damn reassuring to meet pathologist Dr. Lombard, one my my personal hidden heroes, who helped me navigate those critical first days of my diagnosis even though I didn’t realize it until 3.5 years later.
[A huge thank you to Dr. Lombard and the pathology team at El Camino Hospital for your critical role in my care, and your hospitality during my visit.]